Current studies
If you have a study that you would like the RCM to support and host on its website or would like to discuss a forthcoming piece of research, please get in touch via [email protected]. Our Research Advisors Jenny Cunningham and Jude Field are happy to discuss requests. All requests get considered at a meeting of Expert Clinical Advisory Group.
This research impact project aims to assess alternative ways of sharing research findings, specifically through social media campaigns that direct users to a dedicated website detailing the results (see link below).
In 2020, an online UK national survey of midwives working in the NHS was conducted. The survey sought to address a gap in the evidence, specifically how working practices, such as shift length, the ability to take rest breaks, finish shift on time or intershift recovery might influence midwives’ emotional wellbeing. Over 2300 midwives from the four UK nations took part. There were consistent associations between impeded recovery time from current working practices, including a lack of formal methods to monitor this, and poorer emotional wellbeing outcomes that potentially influence midwives’ ability to provide safe and effective care. The findings highlight areas where job design and working practices may be improved, which may contribute to better understanding in staffing and retention strategies.
Whilst key research findings have been published in an open access international peer-reviewed midwifery journal (click here to access), the rise in social media platforms in recent years has introduced innovative methods of dissemination that can reach a wider audience and make the research more visible. An infographic (below) will be used to engage social media audiences across a range of platforms.
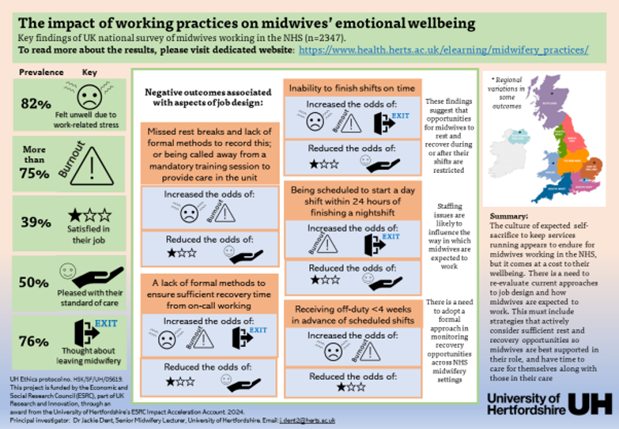
Social media posts will direct users to an interactive website that has been created to share the survey’s findings, highlighting factors related to job design that may influence emotional wellbeing outcomes. Findings are also potentially relevant to other healthcare professionals. The website aims to present a plain English summary of the findings, with easy to navigate expandable links and pop-up boxes that provide more detailed information should users wish to explore further. The website also includes interactive regional map of results and opportunity to provide feedback. Access website on this link
A duplicate copy of the website, with a unique URL has been created for midwifery leaders, specifically seeking feedback to understand whether they would consider modifying policies or aspects related to job design in light of the survey’s findings. This link will be shared by the Royal College of Midwives and circulated through their Director/Heads of Midwifery network, but midwifery leaders can request the unique link by emailing the researcher, Dr Jackie Dent via email [email protected]
This project is funded by the Economic and Social Research Council (ESRC), part of UK
Research and Innovation, through an award from the University of Hertfordshire’s ESRC Impact Acceleration Account. 2024. UH Ethics protocol no. HSK/SF/UH/05619.
Project PI: Dr Jackie Dent, Senior Midwifery Lecturer, University of Hertfordshire.
You can also find me on X @midwifejdent
This is a mixed method PhD study aiming to explore how NHS Trusts in the UK meet the needs of women and birthing people who make birth choices that fall outside of the guidelines and recommended care. The online survey aims to identify and understand current practice and clinical care pathways, challenges, and pave the way for innovative solutions regarding “Out of Guidance Birth Choices” across the country.
You need to be a consultant midwife /consultant midwife in a development role, senior midwife or a midwife assigned to complete the survey who is currently working in the maternity services of the NHS and you are invited to participate in this online survey. Therefore, if you are unable to provide this information, please pass this questionnaire to a more appropriate colleague. Taking part is completely voluntary and should take approximately 15-20 minutes to complete the survey. Rest assured; all responses will be treated with the utmost confidentiality. By contributing to this study, you will play a pivotal role in shaping the future of Out of Guidance birth choice services.
The survey will cover information about your maternity unit, including annual birth numbers, referrals to Out of Guidance birth clinics, Out of Guidance births, and related care policies, so you may want to look at this information before starting the survey.
Upon completing the survey, you will have an option to express your interest to participate in the second phase of the study. The second phase involves qualitative interviews to delve deeper into the standards, processes, and cultural contexts of supporting service users who make birth choices that fall outside the standard patterns of care provision. This phase aims to identify best practices and provide key recommendations for midwifery education and policy development.
If the QR code is not working, you can access the survey here
Should you have any queries or require further information, please do not hesitate to contact me at [email protected]
Facebook: The MIROG Study – UK
Instagram: @midwiferyresearchoog
We are exploring the views and experiences of parents, midwives and doctors in connection with parents’ involvement in decisions about possible planned birth at 34+0-38+6 weeks of gestation.
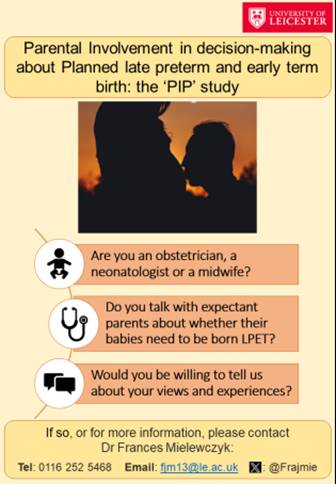
Background
We know little about the input parents would like to have in decisions about the possible planned birth of their babies at late preterm or early term. We also know little about what kind of input midwives and doctors think parents should have. However, we do know that around half of women are dissatisfied with their involvement and that some of these go on to become dissatisfied with their maternity care overall. We also know that the views of midwives and doctors sometimes differ.
We are therefore interviewing those with recent experience of such discussions about their views and experiences and hope that this may help us identify ways that parents may best be supported during the decision-making process.
Who are the research team?
The Principal Investigator on this project, Dr Frances Mielewczyk, is a former paediatric and neonatal nurse now working as a researcher at the University of Leicester. Her work forms part of the Leicester City Football Club (LCFC) Research Programme, which is led by Professor Elaine Boyle, Consultant Neonatologist and LCFC Professor of Child Health, and funded by a generous donation from LCFC.



My name is Helen Parsons and I am a psychology PhD student at Birmingham City University. My topic is health behaviours, body image and mindfulness-based concepts in pregnancy. I want to find out about midwives’ experiences and perceptions of providing support and advice on healthy eating and lifestyle behaviours during pregnancy. I am also interested in their views on how healthy lifestyle services within maternity care could be improved. Given that Black and Asian women are more likely to have adverse birth outcomes compared to white women, I am especially interested to speak to midwives who provide antenatal care to pregnant women from ethnically-minoritised groups. For this study, I would like to talk to NHS midwives who work with women in the antenatal period of any band, in any setting. Third year midwifery students who are working alongside community midwives and who are close to completion of their studies may also be eligible to take part. It will be an opportunity for midwives to tell me about their experiences in this area of antenatal care and input into any recommendations or improvements they would like to see. Participation will involve completing a brief pre-interview questionnaire and taking part in a 30-minute online interview. My supervisors are Professor Helen Egan, Dr Kathrina Connabeer and Professor Michael Mantzios of Birmingham City University.


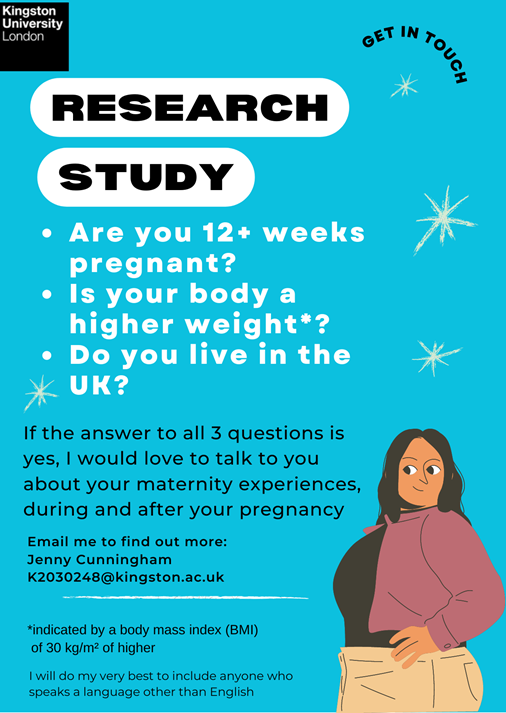
My name is Jenny Cunningham, I am a midwife and am undertaking a part time PhD. My topic is weight stigma in pregnancy and I want to find out more about the experiences of higher weight women and birthing people in the UK and how their care could be improved. I am working with a group of women - the Research Collective - who have had babies as higher weight women and they are advising me and supporting the study. For this study, I would like to talk to women three times, twice in pregnancy and once after the baby is born to ask about their experiences. It will be an opportunity for them to tell me about their maternity care. I am also inviting participants to keep a creative journal and I have some materials to send those who want to do this. My supervisors are Dr Kirstie Coxon of UCLan and Dr Melania Calestani of Kingston University.

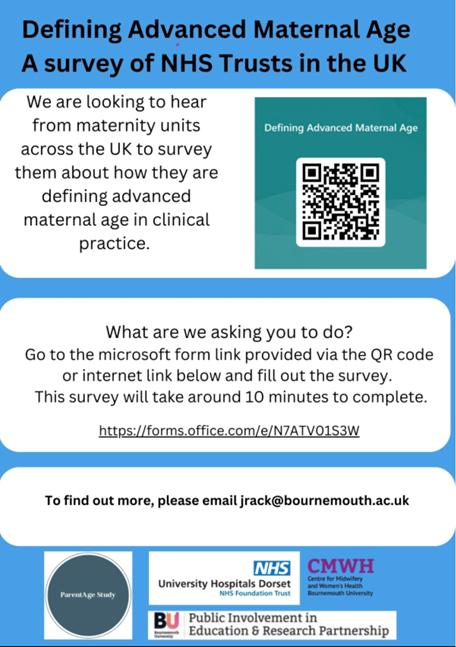
Background:
The proportion of births to women over 35 years of age has increased significantly in the last decade. Care planning for older mothers was highlighted in the 2020 MMBRACE report as an area of concern with recommendations for improvements. However, the definition of advanced maternal age (AMA) varies in the literature. Women's care plans and care pathways are being defined based on these inconsistent parameters. As a method of validation and context for the PhD titled: Personalized care of women of advanced maternal age, it is important to understand how AMA is being defined in practice across the UK and what key documents are being used to guide clinical decision making and care planning.
The objective of the survey is to audit and map current practice across the UK. Identifying current definitions of advanced maternal age (AMA) and applicable clinical practice guidelines/protocols/care pathways used for this demographic of childbearing women. We aim to reach as many NHS Trusts and maternity units as possible to obtain broad information on different UK countries and regions.
We are seeking to answer the question: How is advanced maternal age being defined in practice across the UK today?
Who is the researcher?
Joanne Rack is a Clinical Doctorate student at the Centre for Midwifery and Women’s Health in the Faculty of Health and Social Sciences at Bournemouth University. She is being supervised by Dr. Vanora Hundley, Dr. Edwin vanTelijligen and Dr. Ann Luce. A registered midwife with the Nursing and Midwifery Council (NMC) and with the College of Midwives of Ontario (CMO). She has an MSc. in Reproductive and Sexual Health Research from the London School of Hygiene and Tropical Medicine. As a maternal health researcher and practicing midwife, she sits on the provincial task force for the revision of current provincial clinical practice guidelines on post-partum haemorrhage for the Association of Ontario Midwives and is a research fellow and part time research assistant under Dr. Beth Murray Davis at The McMaster Midwifery Research Centre.
We would be grateful if you would support this research.
Please click here to access the survey.


The care of women with hypertension following maternity discharge is often haphazard, with little evidence to guide best practice. This study aims to understand current postpartum care pathways so that future work to develop an intervention to control BP better will be effective and appropriate for all women and their healthcare teams.
Midwives and MSWs with experience in caring for women with high blood pressure following pregnancy are invited to fill out the survey.
Who’s the researcher?
Katherine Tucker is the lead research fellow and co-investigator on an NIHR programme grant to explore and evaluate a self-management intervention to better control postpartum blood pressure following hypertensive pregnancy.


My name is Eleanor Laidlaw Brown and I am a part time researcher at the University of Huddersfield working towards a PhD in Public Health. I work part time as a health visitor, I am a qualified midwife and I am self-funding my research role. I have been involved with Domestic Abuse services for the last 14 years since leaving a domestic abusive relationship, which also saw me providing education to health professionals.
In my study, I have interviewed women about their experiences of coercive control as part of domestic violence and abuse during the perinatal period (pregnancy, birth and early parenting). I am now aiming to explore the experiences that midwives face when they are supporting women who have been coercively controlled. Once I have all the data from the in-depth interviews with both the women and midwives, I then plan to disseminate the results via a number of platforms including research papers to help health professionals recognise if a woman is experiencing coercive control in the perinatal period.
Victims of coercive control very often cannot see that they are in an environment of abuse especially when there is no physical abuse. This is because many of the tactics and behaviours used are very subtle and happens progressively over time and often in private in own homes. In addition, previous research has found gaps in support from professionals. If health professionals were better able to identify coercive control, they would then be able to help the victim recognise what was happening to them and then be able to offer support and refer on to specialist domestic violence and abusive agencies and services.
I am looking for midwives to take part in individual in-depth semi-structured interviews that I anticipate will take approximately 1 hour. The interviews will be conducted via online platform Microsoft Teams and recorded so that they can be typed up. Click here to download the participant information sheet.
If you would be willing to take part in my research or would like any further information or have any questions then please can you make contact with me by email [email protected].
Thank you for taking time to read this invitation.
If you are a health care professional (doctor, nurse, midwife, or an allied health professional (see list below) working at least one day per week in any healthcare organisation (primary care, community care, care homes, acute care) in the UK, we would love to hear from you.
We are seeking to gain an overview of NMAHPs’ perceptions about their own, their teams, and their organisation’s ability to engage in different levels of research-related activity. You can fill in the survey here.
It doesn't matter if you are already involved in research, or have no experience of research at all - we would like you to share your views.
The survey is led by the University of Sheffield. The study has been reviewed and approved by the ethics committee of the University of Sheffield.

CALLING PARTICIPANTS for research study...
“A mixed method study exploring maternity services and support available within the United Kingdom NHS for women presenting in the antenatal period after previous experiences of self-defined traumatic birth.”
My name is Francesca Marino, a midwife and postgraduate student undertaking a Master (MRes) Degree in Health and Social Care Research from the University of Manchester. As part of my Masters Degree, I am undertaking a project looking at exploring maternity services and support provided to women or birthing people presenting in pregnancy with previous self-defined traumatic birth across Maternity Units in the UK.
The findings will provide valuable information on maternity services available, and the way they are provided and will inform future research, which may include reviewing or developing guidelines or developing standardised and evidence-based interventions with improved outcomes for women and families.
Participation will involve completing an online survey accessible via the link below. The survey is addressed to midwives who can provide information regarding NHS maternity antenatal services and support for women or birthing people with a history of previous traumatic birth. If you are unable to provide this information, please pass this e-mail on to a colleague to complete the survey. We would kindly ask you to ensure only one midwife representative of your maternity unit and Trust completes this survey to avoid obtaining more than one response from the same trust or maternity unit.
We aim to reach as many NHS Trusts and maternity units as possible to obtain broad information on different UK countries and regions.
Please note that the survey will ask for information on the maternity service including the number of births per year at your maternity unit, policy related to care, and pathways for previous experience of traumatic birth, so you may want to look at this information before starting the survey.
The survey will take approximately 15-20 minutes to complete depending on the time you need to gain the information stated above.
At the end of the survey, you will also be asked if you would like to participate in a follow-up interview to explore individual experiences and aspects related to caring for women with a previous traumatic birth, by those who provide the services.
We would be grateful if you could support this research.
Click here to access the survey.
Alternatively, you can scan the following QR code:

Please do not hesitate to contact me at [email protected] or my supervisors
[email protected] or [email protected] if you have any further questions.
Midwives are often expected to work with students in clinical practice, contributing to their education and development, but very little is known about if midwives feel capable and confident performing this role.
This study aims to look at levels of confidence and adaptability (also known as self-efficacy) when working with and teaching student midwives. This anonymous survey should take around 10 minutes to complete.
To participate you need to:
- Be a midwife registered with the Nursing and Midwifery Council
- Have worked as a midwife in the UK within the last year
- Have worked with a student midwife in practice within the last year
If you are eligible please click here to follow the link or scan the QR code on the poster below!
Who is the researcher?
Rosy Jordan is a midwife and Medical and Healthcare Education Masters student at Anglia Ruskin University (ARU). She is also a senior lecturer practitioner at ARU. The supervisor for this project is Dr Sarah Lockey, senior lecturer at ARU School of Medicine.
Melissa Loh is currently in post as an Oral Surgery Registrar working across the University Hospitals of Morecambe Bay NHS Foundation Trust. Allaan Heewa is in his second year as a Dental Core Trainee (DCT) in Paediatric Dentistry working in Barts Health NHS Trust. Both Melissa and Allaan are supervised directly by Mr. Rory Molloy, the Consultant Oral and Maxillofacial Surgeon (OMFS) working in the University Hospitals of Morecambe Bay NHS Foundation Trust with a keen interest in the diagnosis and management of tongue ties in paediatric patients.
This project, ‘Addressing Ankyloglossia’, reviews national data collection from Midwives to identify their incidence regarding their approach to tongue tie referral for release. In addition to analysing their experience with managing referrals into OMFS.
The project aims to review the current practice within OMFS departments across the nation. This includes frequency of tongue tie release, the indications for the treatment and review the overall consensus for active tongue tie release.
To help us develop the national questionnaire, the project aims to identify and understand whether OMFS departments have a dedicated clinic for assessment, and whether the patients are assessed by a qualified feeding specialist prior to referral; is there and age criteria and what is the current consensus in regards to follow up after the treatment.
Healthcare professions must consider a parents’ parent or guardian concerns and expectations during the consultation. By reviewing the current practice across the country, a consideration the development of national guidelines could be of unanimous benefit. This is often an emotive topic particularly when discussing the extent of the associated benefits of a tongue tie release; in particular, in relation to the breastfeeding relationship between mother and child.
The link to our online national survey aimed at healthcare professionals involved in tongue tie release identification and management. We would be grateful if you could spend a few minutes of your time completing this survey which will aid our data collection process. https://forms.gle/FgPXcfH7iP4gi7Uw6
For more information, please contact:
Melissa Loh (Oral Surgery Registrar): [email protected]
The below is an invitation for midwife leaders from Black or Mixed ethnic backgrounds working in the NHS at band 8 and above level to participate in a survey about their work experiences. You can find the survey here.
This survey will be open until July.
Examining the experience of midwives as the second victim after making an error in clinical practice
Are you a midwife?
Have you made an error in clinical practice?
Safety in maternity care is very important. I would like to invite you to take part in an anonymous PhD research study about midwives’ experiences of making errors in clinical practice entitled:
An exploratory study examining the concept of midwives as the second victim. What experience do midwives have as the second victim after making an error in clinical practice? IRAS number 312715.
I would like to find out about your experiences as a midwife if you have made an error in clinical practice with a view to establishing an evidence base for this and recommending a specific evidence-based support system for midwives.
All information collected during the research will be anonymous.
Completing the questionnaire and returning it indicates consent to the study. You can stop being part of the study at any time, without giving a reason, but we will keep information about you that we already have.
As a thank you for your time in taking part, if you complete a separate link available at the end of the questionnaire, with your name and email address you will be entered into a draw to win a £25 Amazon Voucher. You will be notified by email if you have won.
Thank you for your help. Your views are so important to me, midwives’ voices need to be heard.
- Natasha Carr
Find the survey here.
![]()

The Maternal Health and Wellbeing Research Group at the University of Nottingham is undertaking a project to explore implementation of remote/virtual care during pregnancy. The study is called ARM@DA (A Realist Inquiry into Maternity Care @ A Distance) and seeks to understand how digital consultations can work to support safe, personalised and appropriate maternity care and to clarify when they might be most appropriately used, for whom, when, and in what contexts. The 18-month project is being led by Dr Catrin Evans and is a realist review. This type of evidence synthesis incorporates extensive stakeholder engagement (including health professionals, maternity advocacy and community organisations and service users), alongside an in-depth and comprehensive review of the global evidence in this area.
The review output will be a theoretically-grounded explanatory framework for safe, appropriate and acceptable digital consultations in maternity care that can be used by NHS stakeholders to guide future service development, policy, practice and research.
We would love you to get involved in our stakeholder events and webinars. See the ARM@DA project website for more details and to express an interest. Alternatively, drop us an email: [email protected].
Anna Madeley is a Midwife, Lecturer and Doctoral student at the Open University, Faculty of Wellbeing, Education and Language Studies. Her research, writing and academic interests including complex pregnancy planning, home birth and outside of guidelines care.
This grounded theory study PhD aims to improve understanding of and explain why and how women and birthing people make their decisions to make non-normative or alternative choices in pregnancy and childbirth, as well as the underlying social processes that accompany them.
By understanding these experiences and choices, it is anticipated that we can learn more about how we can support as well as align and contrast with existing knowledge around how clinicians support alternative choices to create a firm evidence base upon which to predicate equitable care pathways.
Examples of a non-normative choice in pregnancy and childbirth might be:
- Requested care or place of birth that isn’t routinely offered, recommended, or medically indicated?g., Caesarean Section with no medical or obstetric reason, non-low risk home birth or waterbirth, freebirth (list not exhaustive)
- Declined or refused care or intervention that IS recommended, offered routinelyg., declining pre-pregnancy care or preparation for pregnancy, screening, Induction of labour, vaginal examination, antenatal care, fetal monitoring, screening, clinical examination (list not exhaustive)
This research project has been reviewed by, and received a favourable opinion, from The Open University Human Research Ethics Committee on 10/08/21 – HREC reference number: 4062
To learn more or enquire about taking part, email: [email protected] or follow
T: @NNChoiceProject /@annathemidwife
Instagram: nn_choices_in_maternity_project


Dr Christy Burden and Dr Anna Davies from the University of Bristol and Southmead Hospital (North Bristol NHS Trust), are undertaking a study investigating current and Covid pandemic-related changes in practice for identifying and managing overweight women and women with risk of gestational diabetes (GDM). This work is part of an international trial with colleagues in Australia, Ireland and Spain (Impact Diabetes: URL) in which they are trialing an App-based lifestyle intervention to prevent GDM and reduce maternal weight in pregnancy.
The aim of our survey is to map NHS practice and variations for managing overweight women and identifying and managing women with GDM. We would like staff who have a role in the care of women who are overweight and/or women with GDM to tell us about current practices in their maternity service. Please click on this Survey link, which takes around 10 minutes to complete.
Thank you for your support. Please email [email protected] for any information.



Rachel Rowe is an Associate Professor and Senior Health Services Researcher in the NPEU at the University of Oxford, and the Head of the UK Midwifery Study System (UKMidSS), which she set up in 2015, funded by an NIHR Post-doctoral Fellowship. Her research interests include intrapartum care, the organisation of maternity care and women’s experience of care, with a particular focus on midwifery-led settings. She is also a co-investigator for the NIHR Policy Research Unit in Maternal and Neonatal Health and Care.
The UK Midwifery Study System (UKMidSS) is national system for carrying out research in midwifery units. The UKMidSS Diabetes Study aims to investigate how many women with diabetes (gestational or pre-existing) are admitted to midwifery units for labour care, what the characteristics and outcomes of these women (and their babies) are, and whether some women with diabetes might safely plan birth in a midwifery unit, particularly an alongside midwifery unit where there is ready access to neonatal care.
Ethical review has been obtained from NRES Committee South West – Frenchay
For more information or to discuss participation please visit our website or contact: [email protected].
Twitter: @NPEU_UKMidSS
This survey aims to assess current practice in UK maternity units for the detection of breech presentation at term. Some units are currently offering routine ultrasound scans to all women, or groups of women, to avoid undiagnosed breech presentation during labour. However, the rollout and use of such scanning in the UK is currently unknown. The aim of this survey is to understand how practice differs between NHS Trusts or Health Boards. This information will be helpful to assess the feasibility of implementing ultrasound screening as a tool to diagnose breech presentation at term. The aim is not to promote ultrasound screening at term, but to understand current practice across the UK.
The survey is being carried out by researchers at the University of Aberdeen and Cardiff University. We would be grateful if you could tell us about current practice at your maternity unit by clicking on the link to complete the survey.
Maternity studies with RCM involvement as stakeholders
Avoiding Brain Injury in Childbirth (ABC) project The project focus is on monitoring and responding to babies’ wellbeing during labour and on managing the emergency complication at caesarean section known as impacted fetal head. We are inviting maternity staff, parents and birth partners from across the country to contribute. Please register to take part
Re:Birth The Re:Birth project aims to enable the maternity community across the UK – midwives, obstetricians, service users, support workers, students, researchers and others - to come together to develop a new, shared, positive narrative around birth.
Each year in the UK, 80% of women who give birth vaginally (450,000 women), experience damage to the surrounding area. This may result from tears or cuts to tissues, muscles and skin around the bladder, vagina and perineum (the skin between the vagina and back passage). This is called Childbirth Related Perineal Trauma (CRPT). CRPT needs to be dealt with quickly and effectively. If not treated, women can be left with pelvic floor problems or psychological problems.
The Chapter Study programme involves four interlinked work packages, with patient and public involvement (PPI) throughout, with the aim of standardising and optimising the care of women with CRPT.
The OASI Care Bundle Project The OASI Care Bundle, a joint enterprise between the RCM, the RCOG and LHSTM (London School of Hygiene and Tropical Medicine) with the aim of reducing incidence of OASI. An OASI is an obstetric anal sphincter injury which can occur during vaginal birth, sometimes referred to as severe perineal tearing. The long-term consequences of OASI include anal incontinence and painful sexual intercourse (dyspareunia) which can result in significant emotional and medical impact on women Resources for women with perineal trauma